Abstract
INTRODUCTION: Atypical hemolytic uremic syndrome (aHUS) is a complement mediated thrombotic microangiopathy that predominantly affects the kidneys although extra-renal manifestations are common. In the pre-eculizumab era, 40-65% of patients either died or had end stage renal disease (ESRD) at 1 year. Long-term renal and cardiovascular outcomes are less well described in the eculizumab era. We conducted this cohort study to describe the renal and cardiovascular outcomes of adult survivors of aHUS, both on and off continued eculizumab therapy.
METHODS: Patients with aHUS were identified from the prospective Complement Associated Disease Registry and through the Center for Clinical Data Analysis at Johns Hopkins University. Demographic and clinical data were abstracted, including details of aHUS diagnosis, laboratory studies, treatment, and outcomes including renal function, hypertension and echocardiographic studies. The prevalence of hypertension was compared between patients with and without chronic kidney disease (CKD) using the chi squared test.
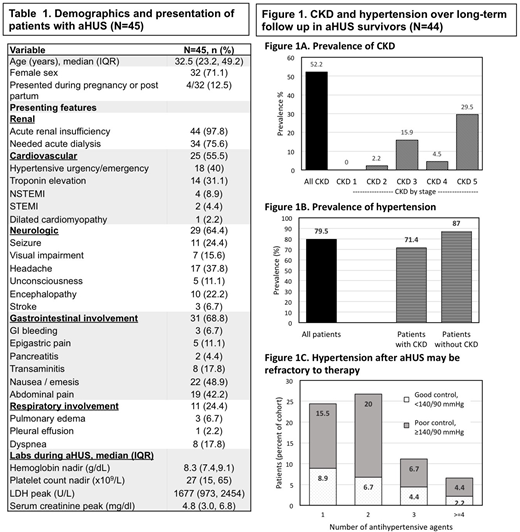
RESULTS: 45 individuals with aHUS were followed at Johns Hopkins Hospital with a median [interquartile range (IQR)] time since diagnosis of 37.4 [IQR 20.7, 62.6] months. Median age at diagnosis was 32.5 [IQR 23.2, 49.2] years and 71.1% were female. Acute kidney injury was present in 98% (44/45); however, neurologic (64.4%), gastrointestinal (68.8%), and cardiovascular (55.5%) involvement was also common (Table 1). Hypertensive urgency or emergency was present in 40% (18/45), while 13.3% (6/45) had an acute coronary syndrome during the acute episode (2 ST elevation myocardial infarctions and 4 non-ST elevation myocardial infarctions). Complement gene sequencing was completed for 34 patients, of which 8 had variants in CFH, one in CFH and CD46, 5 in other genes (MCP1, CFHR1 homozygous deletion, DGKE, THBD, and THBD with del(CFH-SCR20-CFHR1-int5)]and 20 patients had no pathogenic variants. Thirty-two (71.1%) patients were treated initially with plasma exchange (median 6 [3, 12] exchanges). Thirty-nine (86.7%) received eculizumab (5 started at the time of renal transplant after developing ESRD), and 20 of these (51%) have since discontinued therapy. Median duration of eculizumab therapy was 2.7 [0.9-11.3] months for those who stopped therapy and 29.5 [8.8-55] months for those who continued. One patient died due to a myocardial infarction during the aHUS episode.
Of the 44 survivors, 15 (34.1%) had complete renal recovery, 9 (20.5%) had chronic kidney disease (CKD) stage 1-4, and 20 (45.5%) developed CKD stage 5 requiring dialysis at 3 months after the acute episode. Fifteen patients underwent subsequent renal transplantation. At the end of follow up, 23 (52.2%) had CKD [2.2% stage 2, 15.6% stage 3, 4.4% stage 4 and 28.9% stage 5) (Figure 1A). Although not statistically significant, there was a higher rate of CKD (63.1% versus 52.6%, P=0.511) among those not on eculizumab; however, this primarily reflects eculizumab being stopped after ESRD. Hypertension was present in 35 (79.5%) survivors (Figure 1B), of which 14 (40%) had incident hypertension. The prevalence of hypertension was not significantly different between patients with CKD and normal renal function (87% versus 71.4%, P=0.202). Thirty-one (70.4%) were on antihypertensive therapy, and 67% (21 of 31) of these were not controlled to <140/90 mmHg despite the use of multiple agents (Figure 1C). Echocardiograms were performed in 29 (64.4%) individuals (12 within 3 months of diagnosis, and 17 after 3 months). Of these 17, 29.4% were normal studies, 23.5% had reduced left ventricular ejection fraction, 29.4% demonstrated left ventricular hypertrophy or diastolic dysfunction, and 11.7% had pulmonary hypertension.
CONCLUSION: Malignant hypertension and cardiac involvement are common during acute aHUS. aHUS survivors also have a high prevalence of hypertension, including a notable incidence of new onset as well as uncontrolled hypertension following aHUS diagnosis. CKD is present in the majority of survivors, and structural cardiopulmonary disease is common. Complement activation has been implicated in the pathogenesis of cardiovascular disease. Further investigation is needed to evaluate the epidemiology of cardiovascular sequelae in aHUS, their associations with specific complement mutations, and optimal management.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal